 An immune response can be helpful, harmful, or somewhere in between, in COVID-19 and many other medical conditions.
An immune response can be helpful, harmful, or somewhere in between, in COVID-19 and many other medical conditions.
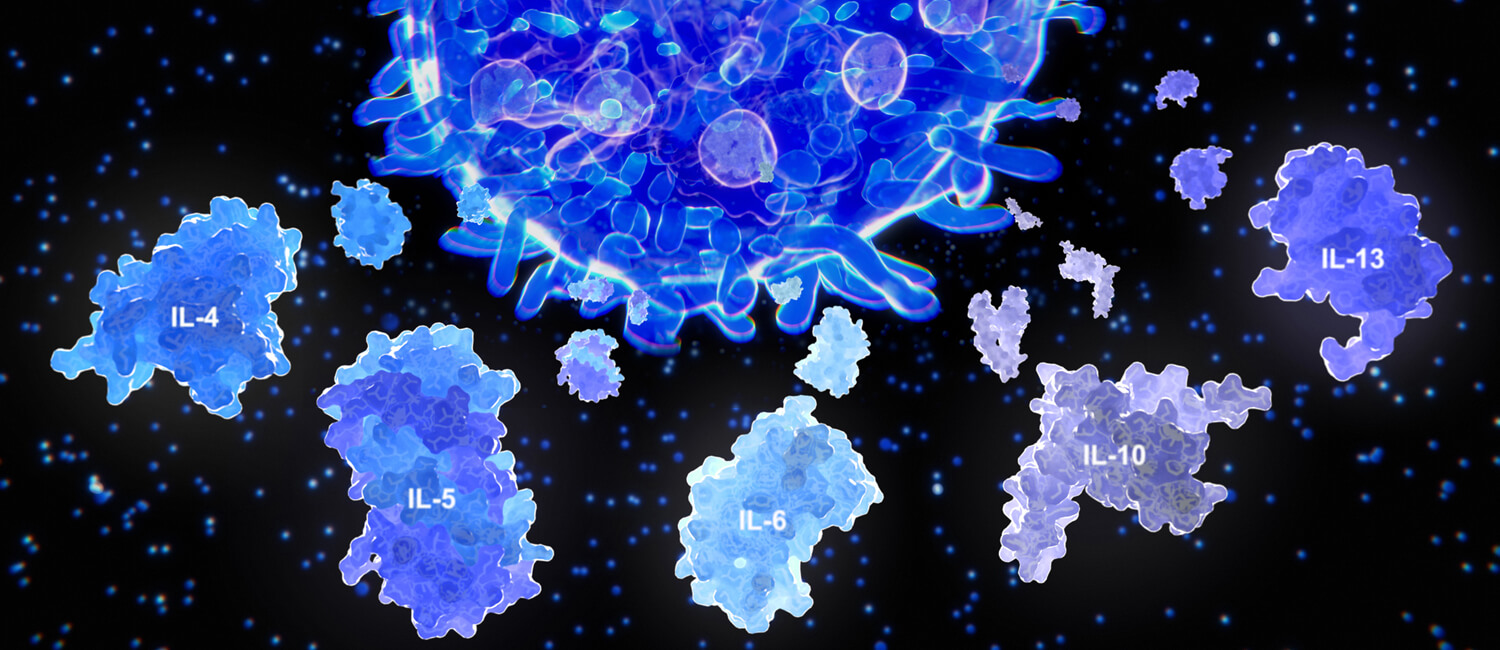
While countless mysteries remain regarding COVID-19, some clinicians and scientists have come to believe that some of the worst effects of the disease — from respiratory difficulties to organ damage — are the outcome of a cytokine storm, an onslaught of immune activity that veers out of control, causing serious harm or even death.
With a mutual interest in immunology — both its helpful and harmful aspects — Dr. Christopher Hunter, Mindy Halikman Heyer President’s Distinguished Chair of Pathobiology at Penn Vet, and Dr. Nilam Mangalmurti, Assistant Professor of Medicine and attending physician at the Perelman School of Medicine (PSOM), found they had a lot to discuss after colleagues introduced them two years ago. Their shared interest has gained a new relevance during the pandemic, and they recently teamed up to write a primer on cytokine storms for the journal Immunity. Here they answer questions about what they’ve learned.;
Q: How do you define cytokine storm and sepsis?
Hunter: Everyone has cytokines circulating in their bodies; that’s a normal part of the immune response. But when that response overshoots where it should be to clear an infection, that’s where it becomes pathological and is considered a “storm.” And it doesn’t have to be an infection that triggers it. It could be that something turns on a T cell by mistake, it could be an autoimmune response, or it could be a treatment that boosts the immune response to cure cancer.
Mangalmurti: Sepsis is now defined as an abnormal host response to a pathogen, whether it’s bacteria, virus, parasite, or fungi. Most people should be able to clear the pathogen and return to a normal state. Sepsis is a dysregulated response where there is not necessarily a return to normal. In sepsis, the response is often characterized by a hyperinflammatory and an immunosuppressive response happening at the same time. Hunter: A cytokine storm can be part of that. The question is, “At what point does cytokine activation become pathological?”
Q: How is what we’re seeing with COVID-19 confirming or changing what we understand about cytokine storms and how to address them in patients?
Mangalmurti: One thing that was very clear to us after the first week of seeing COVID-19 patients was that most who came into the ICU with organ failure clearly had a condition that seemed to predispose them to vascular injury: obesity, diabetes, high blood pressure, age, a history of vascular disease, or clots. And that was striking because it’s not something we usually see in most other forms of sepsis, or other forms of acute respiratory distress syndrome.
That got us thinking about innate immunity in the vascular compartment and whether this virus had a penchant for the vasculature. Maybe there’s a way to use what we know about this relationship with the vasculature to design and use more targeted anticytokine therapies.
Hunter: From my perspective it’s exciting to think about targeted therapies that are already available, like antibodies to cytokines that are already used in the clinic; maybe they could be repurposed and used in this setting. But we really need large clinical trials to assess whether our excitement about some of these approaches is meaningful and valid.
Q: Your work seems to underscore the value of collaboration across fields.
Hunter: Absolutely. Nilam has worked on sepsis and has been seeing sepsis patients for a long time. She’s dealing with really sick patients who have a lot going on. Basic scientists tend to want to simplify and reduce things. And you’ve got to meet somewhere in the middle, I think, for complex diseases. Penn is a really good place to do that, at PSOM, CHOP, and Penn Vet.
For a longer interview, read the Penn Today story.