Dr. Andrew Vaughan is an assistant professor (tenure track) in the Department of Biomedical Sciences. Dr. Vaughan received a B.S. in Biochemistry from the University of Nebraska before earning his Ph.D. in molecular and cellular biology from the University of Washington. In Seattle, he worked with gene therapy pioneer Dr. Dusty Miller at the Fred Hutchinson Cancer Research Center. Having gained an interest in pulmonary regeneration due to his work with the Jaagsiekte retrovirus, a causative agent of lung cancer in sheep, Dr. Vaughan pursued a postdoctoral fellowship with Dr. Hal Chapman at the University of California San Francisco, studying somatic stem cells and lung injury repair.
How do we think about regenerative medicine?
In a 2001 episode of South Park, the ever-scheming Eric Cartman plots to obtain large quantities of embryonic stem cells through nefarious means. His ultimate goal—to clone his favorite restaurant, Shakey’s Pizza. While an obviously absurdist take on the potential of stem cell therapy, the biomedical community has been dogged by similarly simplistic notions of how cell therapy might work. Countless studies have claimed that injecting ill-defined “stem cells” into a damaged tissue will regenerate that organ or otherwise provide therapeutic benefits. The existence of clandestine “stem cell clinics” further cements these unrealistic expectations of stem cell-based therapies.
While stem cells are often considered essential for regenerative medicine, many of our fully developed somatic tissues already possess great capacity for regeneration. Indeed, the liver has been recognized as especially regenerative since Classical Greece, and similar reparative properties of the intestine and epidermis are well known. Based on his interest in lung injury repair, the Vaughan laboratory set out to determine if they could capitalize on these inherent capabilities, harnessing and directing the preexisting capacity for adaptive repair.
Influenza presents a particular challenge for lung repair, given that large regions of epithelium are completely destroyed by infection1. Nonetheless, many (but not all2-4) people recover completely, highlighting a previously under-appreciated capacity of the lung for repair. However, lung regeneration turns out to be quite complex at the cellular level and involves multiple players. While still a postdoc, Dr. Vaughan identified a rare progenitor cell type, similar to basal cells in the upper airway, that expands dramatically to re-cover the denuded alveoli in heavily injured areas 5, 6. While highly migratory and proliferative, these cells (marked by cytokeratin 5 expression [krt5]) do not restore function to gas-exchanging alveoli. Current models recognize these dysplastic cells as an effective emergency response7, but their long-term persistence is maladaptive, and is likely the source of so-called “bronchiolization and “honeycomb cysts” in patients with interstitial lung diseases / fibrosis6.
Notably, other progenitor cells in the lung are much more effective at reconstituting function in regenerating alveolar epithelium. Alveolar type 2 cells (AT2s) are abundant in normal lung, where they produce the surfactant necessary to keep alveolar surface tension low, reducing the work of breathing. AT2s have been long recognized as resident progenitor cells, capable of self-renewal and differentiation into the gas-exchanging type 1 cells8. These cells are also lineage restricted, as Dr. Vaughan’s fate mapping analysis showed that they are unable to give rise to the aforementioned dysplastic cell types. Therefore, “euplastic” regenerative responses from AT2 progenitors are generally beneficial for recovery. Unfortunately, given that AT2 cells are a direct target of many lung injuries, their regenerative capacity can be overwhelmed.
Recognizing the limitations of endogenous AT2s, Dr. Vaughan’s group proceeded to artificially supplement this key progenitor population after H1N1 influenza infection. Utilizing an orthotopic lung transplantation assay, they showed that transplanted healthy AT2 cells proliferated dramatically and retained their AT2 identity, exhibiting efficient euplastic differentiation. This even resulted in improved gas exchange capacity, as measured by pulse oximetry, despite the low engraftment rate of transplanted cells. Dr. Vaughan is currently determining the transcriptional repertoire of these transplanted cells to identify key genes involved in their successful engraftment. By deciphering this “engraftome”, the Vaughan lab hopes to identify target genes that could be modulated to enhance the progenitor cell potential of native AT2s to promote more effective regeneration.
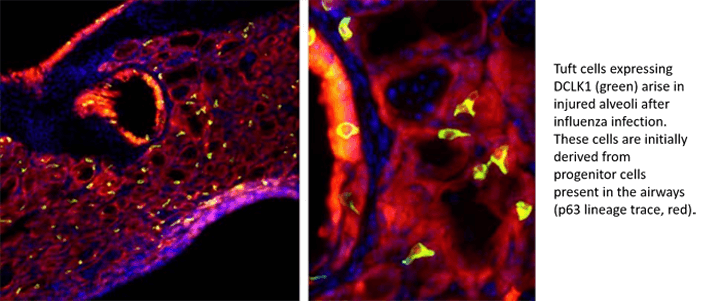
Dr. Vaughan’s laboratory is also interested in the dysplastic “emergency” regeneration that occurs after influenza. While examining the persistence of the Krt5+ cells, they noticed that many of these cells differentiate into solitary chemosensory cells (SCCs), AKA tuft cells. While SCCs were first observed nearly 100 years ago, they have only been recently recognized as the sole source of an important cytokine, IL-25, required for type 2 inflammation, the immune response associated with parasite infections and allergic asthma. Curiously, they are essentially identical to type 2 taste bud cells, utilizing taste sensing “gustatory” pathways to detect molecules associated with various pathogens.
SCCs are absent from the lung in naïve mice, but are normally present in the nasal passages and small intestine, where they are central mediators of both immunity and tissue remodeling / differentiation. Using compounds that exclusively activate tuft cells, Dr. Vaughan showed that injured lungs containing SCCs exhibit acute inflammation upon stimulation. Moreover, administration of these ligands promoted the appearance of even more tuft cells, indicating the presence of a feed-forward loop. Based on tuft cell-mediated metaplasia in the small intestine, the Vaughan lab predicts that these ectopic tuft cells perpetuate the surrounding dysplastic epithelium. These initial studies were recently published in the American Journal of Physiology – Lung Celular and Molecular Physiology, and were highlighted on the NIH Director’s Blog, https://directorsblog.nih.gov/ tag/tuft-cells/
Taken together, Dr. Vaughan’s work reveals that the contribution of competing subtypes of stem/ progenitor cells result in qualitatively and functionally disparate outcomes of regeneration. To return to the South Park anecdote, instead of crudely injecting cells into diseased tissues, Dr. Vaughan hopes to identify environmental cues and paracrine signals that empower the regenerative properties the lung already possess to therapeutically minimize dysplastic responses while maximizing adaptive regenerative pathways that restore function. Cloning a pizza parlor in the process will just be considered an extra perk! Dr. Vaughan’s research is funded by the NIH/NHLBI (R00HL131817) and the Landenberger Research Foundation. His laboratory is located in the Old Vet Building 366E and his office in 370E.
References
- Loosli, C.G. et al. The destruction of type 2 pneumocytes by airborne influenza PR8-A virus; its effect on surfactant and lecithin content of the pneumonic lesions of mice. Chest 67, 7S-14S (1975).
- Liu, W., Peng, L., Liu, H. & Hua, S. Pulmonary Function and Clinical Manifestations of Patients Infected with Mild Influenza A Virus Subtype H1N1: A One-Year Follow-Up. PLoS One 10, e0133698 (2015).
- Koppe, S., Túlio, A.I.B., Villegas, I.L.P. & Motter, A.A. Pulmonary function in patients with pandemic H1N1. Fisioterapia em Movimento 29, 805-812 (2016).
- Chen, J. et al. Long term outcomes in survivors of epidemic Influenza A (H7N9) virus infection. Sci Rep 7, 17275 (2017).
- Xi, Y. et al. Local lung hypoxia determines epithelial fate decisions during alveolar regeneration. Nat Cell Biol 19, 904-914 (2017).
- Vaughan, A.E. et al. Lineage-negative progenitors mobilize to regenerate lung epithelium after major injury. Nature 517, 621-625 (2015).
- Zuo, W. et al. p63(+)Krt5(+) distal airway stem cells are essential for lung regeneration. Nature 517, 616-620 (2015). 8. Evans, M.J., Cabral, L.J., Stephens, R.J. & Freeman, G. Transformation of alveolar Type 2 cells to Type 1 cells following exposure toNO2.Experimental and Molecular Pathology 22, 142-150 (1975)