One Tiny Dog’s Outsized Contribution to Brain Surgery
Geddy Lee has lived a big life for a little dog. As a puppy, the tiny terrier mix was abandoned in Mississippi during a high-speed car chase. Rescued by law enforcement, she found a loving home in Pennsylvania. Life was good—until last summer.
In August, Geddy Lee began having seizures, and her veterinarian referred the eight-year-old to Penn Vet for further evaluation. At Penn Vet’s Ryan Hospital, Tessa Arendt, DVM, specialty intern in Neurology, and Wojciech Panek, DVM, DACVIM, assistant professor of neurology and neurosurgery in the Department of Clinical Sciences and Advanced Medicine, performed a brain MRI, which revealed a right frontal lobe mass.
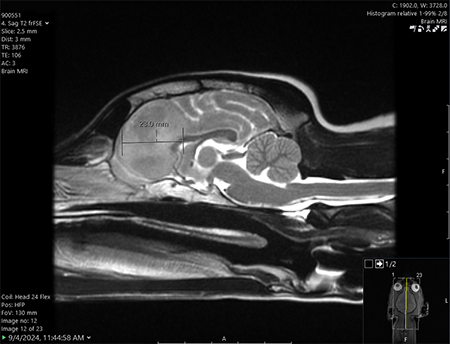
“An MRI doesn’t always tell us exactly what we’re dealing with even though it allows us to see the tumor,” said Panek. “Based on Geddy Lee’s tumor imaging characteristics, we suspected a glioma—an aggressive brain tumor.”
Gliomas affect both dogs and humans. In people, the most malignant type, glioblastoma, carries a life expectancy of approximately 15-18 months with surgery, radiation, and chemotherapy. Without aggressive treatment, dogs typically survive for about a few months.
Geddy Lee’s owners, Michael and Erica Crotty, wanted every option explored, including surgery. Surgery would also enable Panek to biopsy the tumor for a more exact diagnosis and to guide further therapeutic opportunities for Geddy Lee.
“It was amazing how much the team—all the doctors and nurses —rallied around her,” said Crotty. “It was so impressive that they pulled out all the stops, and Erica and I said do whatever you can for our girl.”
Little Brain, Big Impact
Geddy Lee’s procedure took place in September. She arrived at Ryan Hospital on a Monday. A week later, she would leave the first dog to undergo successful canine brain surgery using cutting-edge augmented reality technology combined with infrared real-time guided resection.
Her case required a highly specialized team, including a veterinary neurosurgeon, radiologist, anesthesiologist, pathologist, nurses, and operating room technicians.

Presidential Associate
Professor of Neurosurgery
Joining the Penn Vet experts was a renowned neurosurgeon and brain tumor specialist from Penn’s Perelman School of Medicine: Presidential Associate Professor of Neurosurgery Nduka Amankulor, MD, chief of neurosurgical oncology, and director of the Penn Brain Tumor Center.
Amankulor and Panek partnered on Geddy Lee’s case, merging world-class expertise in human and canine neurosurgery to push the boundaries of veterinary and human medicine.
“When I started at Penn, I approached Nduka because we face similar challenges,” said Panek, who has shadowed his colleague in human surgeries.
Added Amankulor, “One of the things that’s fascinating from a science perspective is that dogs develop brain tumors in a way that’s similar to humans, and genetically, the distribution of brain tumors in dogs is identical to humans.”
“This makes cases like Geddy Lee’s incredibly valuable for both veterinary and human science to advance the care mutually,” said Panek.
A Three-Pronged, Groundbreaking Approach

tools to ensure precise debulking.
The primary goal of cancer excision—or debulking—surgery is to achieve “clean margins.” Even the tiniest remnant of cancerous tissue can increase the risk of local recurrence and disease spread, but gliomas infiltrate healthy brain tissue, making it extremely difficult to distinguish the tumor border.
Geddy Lee’s care team used a combination of advanced tools to ensure precise debulking.
“We combined several novel techniques to achieve the best possible tumor resection,” said Panek. “This was a unique three-part approach.”
A day before surgery, the pup received an injection of a special dye that glows under near-infrared light and accumulates in cancer cells. The imaging agent helps neurosurgeons better identify the limits of the glioma. Penn Vet’s David Holt, BVSc, professor of surgery, developed this technique to remove mammary and lung tumors from dogs.
The next day, Geddy Lee was placed under general anesthesia. The team performed a modified trans-frontal craniotomy, opening her skull for access to the brain. They then used three critical tools for guidance.
“GPS” Navigation for the Brain
First, the surgical team broke new ground by employing an immersive augmented reality neuro-navigational system called VisAR to obtain optimal access to the tumor.
Developed by Novarad Corporation, the technology is used in human medical procedures for its precision and accuracy. It’s essentially, as Novarad describes it, “like a surgical GPS providing a road map to guide the surgeon through simple or complex surgeries.”

an immersive augmented reality tool.
“The technology created a hologram from Geddy Lee’s initial MRI, which was really helpful for procedure planning and navigating hard-to-see areas,” said Panek. By superimposing Geddy Lee’s MRI images with anatomical accuracy onto the dog’s skull, the surgeons were able to first biopsy and then debulk the tumor.
“Penn Vet was the first in the world to use this technology in a canine surgery,” said Novarad CEO Wendell Gibby, MD, the co-inventor of VisAR who trained in neuroradiology at Penn Medicine.
“Unlike traditional navigation, this system doesn’t just project an image on a 2D screen—it places the surgeon inside a fully immersive, 3D anatomical space co-registered to the patient. You can see areas inside the patient that you can’t see with the naked eye; hence augmented reality. The small footprint and lower cost mean that this technology can be widely used by veterinarians everywhere.”
Next for Geddy Lee was infrared imaging: “We shined an infrared camera on the brain, picking up the dye to map the tumor as we operated,” said Panek.
“Because infrared imaging is still relatively new, we also integrated intraoperative ultrasound,” he said. “This enabled us to see into the brain in real-time and confirm the infrared imaging was accurate and that we were removing the tumor to the best of our ability.
”The complex and delicate procedure took roughly five hours and was a success. Geddy Lee emerged from surgery unaware she had just made history.
“The way we approached her surgery highlights the value of state-of-the-art treatments that combine VisAR-guided biopsy and resection with infrared tumor imaging and complex genetic testing to guide the best next therapeutic steps,” said Panek.
The Penn Vet lab of Timour Baslan, PhD, would then perform a whole genome sequencing of Geddy Lee’s tumor.
“In veterinary medicine, the diagnostic process often ends after MRI imaging, and further treatment may be recommended based on those results alone. Many owners opt for radiation therapy or chemotherapy based on MRI findings, but without precise knowledge of the condition, these may not always be the best options.”
Remarkable Dog, Remarkable Recovery
The following day, Geddy Lee was awake and charming her care team.
Soon after, she was discharged with medication to manage inflammation and prevent seizures. Follow-up visits showed she was healing well. During a March re-evaluation at Ryan Hospital, Panek and Arendt were happy to report that Geddy Lee showed no radiological signs of tumor regrowth. Even better was the biopsy result from the Baslan lab.
“Geddy Lee’s genetic testing does not look like it is a glioma,” said Panek. “This is great news for the Crottys!” And for Geddy Lee, who will forever be a veterinary pioneer.
“In human medicine, we often have clearer answers because of extensive research and data. But in veterinary medicine, we are still building our knowledge. Cases like Geddy Lee’s help validate our approach and provide insights for future studies in dogs and humans,” said Panek.
For the Crottys, Geddy Lee’s contribution to science is a value-add: “She’s such a part of our family. There was never a question—we would do whatever it took to help her. And seeing her now, it was all worth it. She’s been through so much, and she just keeps going. She really is a survivor. We’ll always be grateful to the Ryan Hospital team. And we hope that research and technologies that come from Geddy Lee’s surgery can help, even if in a small way, to treat brain cancer.”

Another twist in Geddy Lee’s story: she’s named after the lead singer of the band Rush, whose bandmate Neil Peart passed away in 2020 from brain cancer.
And for Amankulor, the entire experience was more than a professional highlight; it was personal. His father also died of the disease, inspiring him to move the needle on research. And, as a dog owner himself, he felt a personal tug during Geddy Lee’s surgery. “This was one of the most remarkable cases of my career,” he said. “I was emotional when Geddy Lee woke up, knowing what she means to her family. And her case is the beginning of something remarkable for science. It’s powerful, and we should all be proud of her contributions!”
More from Bellwether

In the Office with Donna Kelly, DVM, MASCP, DACPV, DACVPM
Donna Kelly, DVM, MASCP, DACPV, DACVPM, shares her New Bolton Center office with the campus’s microbiology reference library.

Breaking New Ground: Penn Vet Builds Future-Ready Learning Hub
Set to open in the coming months, the 11,800-square-foot clinical skills center will be the first dedicated classroom space on the Kennett Square campus, ushering in a new era of…
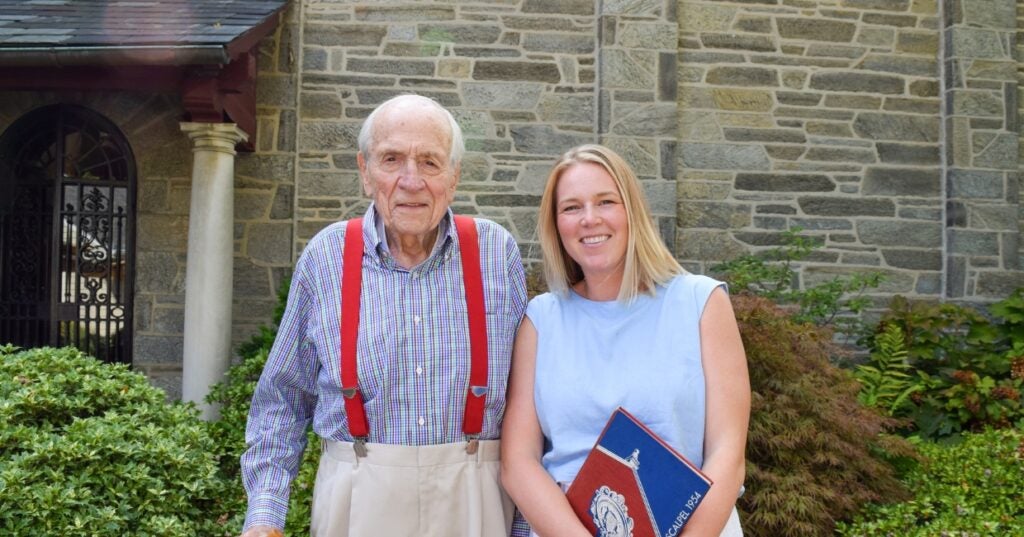
A Love of Animals and the Land
The Penn Vet of Dean Snyder, V’54, was a very different place than today. So was the world.

