Autoimmunity and Inflammation
Antibodies are proteins made by our immune cells, which can recognize infectious organisms and target them for destruction. However, in autoimmune diseases such as systemic lupus erythematosus (SLE), myasthenia gravis (MG), pemphigus, and autoimmune hemolytic anemia (AIHA), antibodies are made against healthy cells of the body and they lead to immune destruction of those cells.
The clinical signs of the autoimmune disease depend on what cells in the body are targeted by the antibodies. Current therapies to treat these diseases in human and veterinary medicine involve using drugs that cause global immune suppression (e.g., corticosteroids, cyclosporine, mycophenolate, etc.). However, these drugs can have unacceptable side effects when used long term, so alternative treatments are being investigated. Cellular therapies and therapeutic monoclonal antibodies are now being investigated that target B cells and plasma cells that produce antibodies. These therapies are changing the landscape of treatments and outcomes for autoimmune disease and much of this work is being performed at the University of Pennsylvania.
At Penn Vet, we are exploring the potential to use plasmapheresis, monoclonal antibodies, and cellular therapies to treat autoimmunity.
Autoimmune diseases such as systemic lupus erythematosus, myasthenia gravis, pemphigus foliaceous, pemphigus vulgaris, autoimmune mediated hemolytic anemia, and immune mediated thrombocytopenia are caused by antibodies generated against proteins expressed on the cell surface or within cells. Current therapies to treat these diseases in veterinary medicine involve using drugs that cause global immune suppression (e.g., corticosteroids, cyclosporine, mycophenolate, etc.). However, these drugs can have unacceptable side effects when used long term, so ongoing Penn Vet research explores the use of cellular therapies to treat autoimmunity.
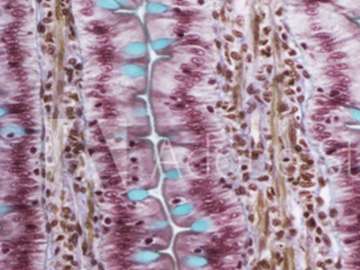
Autoimmune diseases such as systemic lupus erythematosus (SLE), myasthenia gravis (MG), pemphigus, and autoimmune hemolytic anemia (AIHA) occur when your immune system attacks your own healthy cells and tissues. The clinical signs of autoimmunity depend upon which organs and tissues are being attacked. For example, when your immune system targets and destroys red blood cells it will cause anemia, and when it destroys the intracellular “cement” that holds cells within the epidermis (skin) together, it leads to blistering skin diseases such as pemphigus vulgaris.
Autoimmunity is a multi-factorial disease where genetic, environmental, and hormonal influences can all contribute to the generation of auto-antibodies and their ability to cause clinical disease. The triggers are often unknown, but in human patients, flare-ups of autoimmune diseases can occur during or after infections such as a common cold or flu, which activate the immune system.
The most common treatment for autoimmunity is immune suppression. This is achieved by using immune suppressive drugs such as prednisone, cyclosporine, or cytotoxic drugs that prevent immune cells, such as B and T cells from proliferating. More recently, drugs known as small molecule inhibitors, and therapeutic antibodies that inhibit or eliminate B cells that produce auto-reactive antibodies have been used in human autoimmune diseases.
Current therapies to treat autoimmune diseases consist of drugs that cause global immune suppression. They most commonly inhibit the proliferation of B and T cells that make up a large part of the immune system. Global immune suppression can predispose patients to developing infectious diseases. The drugs themselves can have side effects such as gastrointestinal upset, vomiting, diarrhea, increased thirst, increased urination, and weight gain.
Other treatments for autoimmunity aim to inhibit or eliminate B cells and plasma cells — the cells that produce antibodies, including the autoantibodies that cause autoimmune disease. Some of the more recent approaches to treat autoimmunity include the use of drugs that specifically inhibit B cells from proliferating: monoclonal antibodies that inhibit or deplete B cells (rituximab, tafasitumab) and genetically engineered T cells that are programmed to deplete B cells. These approaches are actively being explored in human patients with autoimmunity and the development of biosimilars for veterinary medicine may soon help improve outcomes for dogs with similar diseases.
