Puré Laboratory
Our research focuses on the cellular and molecular basis of inflammation and fibrosis. The Puré Laboratory has made seminal contributions to our understanding of the roles of stromal cells and extracellular matrix remodeling in tissue fibrosis and in cancer risk, initiation, progression, and metastasis.
Our Research

The Puré laboratory is studying the cellular and molecular basis of inflammation and fibrosis that underpin a majority of chronic diseases. We use state-of-the-art multi-omic, genetic, pharmacologic, biochemical, biophysical, and advanced imaging approaches to study the cross-talk between multi-component systems and the mechanisms by which such complex communications networks contribute to pathologic tissue fibrosis and cancer. Our studies encompass the contributions of both tissue/tumor microenvironmental niches as well as systemic interactions that define the host ecology.
An important perspective of our studies is on the essential roles of stromal cells and extracellular matrix (ECM) and their cross-talk with other tissue/tumor components including malignant epithelial cells, endothelial cells, vasculature, inflammatory cells, and immune cells. The Puré lab has made seminal contributions to this field. We have contributed to defining the phenotypic and functional heterogeneity of activated fibroblasts in the context of fibrosis and amongst cancer-associated fibroblasts (CAFs) in solid tumors, as well as the drivers and consequences of distinct activated fibroblast subpopulations. We have established that CAFs regulate tumor growth through both immune-dependent and immune-independent mechanisms. Specifically, we have defined a pro-tumorigenic subpopulation of CAFs defined by their expression of Fibroblast Activation Protein (FAP) and demonstrated that FAP+-CAFs promote tumor growth directly, through dynamic matrix remodeling and by inhibiting endogenous anti-tumor immunity. We have also demonstrated that FAP+-CAFs can render various types of solid tumors resistant to immune checkpoint inhibition and adaptive CAR T cells therapies at three levels:
- by restricting T cell extravasation and tumor infiltration through their roles in disrupting vascular integrity and in perivascular fibrosis in “immune desert/cold” tumors;
- by mediating “immune-exclusion” to prevent access of infiltrated T cells into tumor nests; and
- by mediating immune-suppression.
Based on these results, together with a multi-disciplinary team of investigators (including Drs. Steve Albelda, Carl June, John Epstein, Drew Weissman and many others) at the University of Pennsylvania, we developed FAP-directed chimeric antigen receptor (CAR) T cell therapy for the treatment of solid tumors and fibrotic diseases. Having established proof-of-principle in pre-clinical models of solid tumors (eg. pancreatic, mesothelioma, and lung), and cardiac fibrosis, we are currently conducting IND enabling studies to proceed to clinical trials employing in-vitro generated virally transduced FAP-CAR T cells and/or mRNA loaded targeted-LNPs for in situ generation of FAP-CAR T cells, in combination with vaccines, tumor associated antigen-directed immunotherapies, chemotherapies, and targeted therapies.
In collaboration with Dr. Mark Sellmeyer at Penn, we are establishing FAP-specific PET imaging to screen patients for FAPhi tumors as an enrollment criterion, and to non-invasively assess treatment efficacy in planned clinical trials, for which we have published proof-of-concept in pre-clinical models.
Pre-clinical Models

The Puré lab continues to define novel molecular pathways involved in stroma-dependent tumor growth and fibrosis with the goal of refining therapeutic targeting of stroma in fibrosis and solid tumors, to a molecular rather than cellular level as an alternative approach. The overarching goal of ongoing and studies planned for the foreseeable future is, to define molecular pathways underlying stroma-dependent regulation of anti-tumor immunity, that determine the efficacy of immunotherapies and immune-independent mechanisms by which stroma regulates tumor growth, with a strong focus on normalizing fibrotic tissue/tumor microenvironments.
Collectively, studies in the Puré lab over the next five years will help build a comprehensive understanding of the role of stroma in fibrosis and desmoplastic solid tumors. Any novel mechanisms defined will be evaluated as potential therapeutic vulnerabilities. Candidate targets will inform the future development of novel therapeutics designed:
- to maintain fibroblasts in a relatively quiescent state;
- to inhibit programming of progenitors to pathogenic activated fibroblasts including, targeting ECM remodeling that modulates stiffness that in turn regulates recruitment and/or behavior of virtually all cell types;
- to inhibit the pathogenic effector mechanisms of activated fibroblasts at a molecular level.
Publications
Desmoplastic stroma restricts T cell extravasation, immune exclusion and immunosuppression in solid tumors. Xiao, Z., L. Todd, L. Huang, L, E. Noguera-Ortega, Zhen, L. Huang, M. Kopp, Y. Li, N. Pattada, W. Zhong, W. Guo, J. Scholler, M. Liousia, C.-A. Assenmacher, C.H. June, S.M. Albelda and E. Puré. 2023. Nature Comm. https://doi.org/10.1038/s41467-023-40850-5.
Defining Immune Exclusion: Results of a modified Delphi Workshop. Clifton, G.T., M.L. Rothenberg, P. Ascierto, G. Begley, M. Cecchini, P. Eder, F. Ghiringelli, A. Italiano, M. Kochetkova, R. Li, F. Mechta-Grigoriou, S. Pai, P. Provenzano, E. Puré, A. Ribas, K.A. Schalper, W.H. Fridman. 2023. J. Immunother. Cancer. 11:e006773 doi10.1136/jitc-2023-006773. PMID 37290925 PMCID:PMC 10254706.
Tumor-derived small extracellular vesicles inhibit the efficacy of CAR T cells against solid tumors. Zhong, W., Z. Xiao, Z. Qin, J. Yang, Y. Wen, Z. Yu, Y. Li, N.C. Sheppard, S. Fuchs, X. Xu, M. Herlyn, C.H. June, E. Puré and W. Guo. 2023. Cancer Res. 83:2790-2806. PMID:37115855.
Mechanisms of PDAC subtype heterogeneity and therapy response. In Press. Trends in Cancer. Espinet, E., L. Klein, E. Puré and S.K. Singh. 2022. 8:1060-1071. PMID: 36117109.
Monitoring therapeutic response to anti-fibroblast activation protein (FAP) CAR T cells using [18F]AIF-FAPI-74 PET. Lee, I., E. Noguera-Ortega, Z. Xiao, L. Todd, J. Scholler, D. Song, M. Liouisa, K. Lohith. K.Xu, K. Edwards, M. Farwell, C.H. June, S. Albelda, E. Puré and M. Sellmyer. 2022. Clinical Cancer Research. 28:5330-5342. PMID: 35972732; PMCID: PMC9771904 (available 2023-06-15).
A stromal integrated stress response activates perivascular cancer-associated fibroblasts to drive support angiogenesis and tumor progression. Verginadis, I.I., H. Avgousti, J. Monslow, G. Skoufos, F. Chinga, N.M. Leli, I.V. Karagounis, B.I. Bell, A. Velalopoulou, C.S. Salinas, V.S. Wu, Y. Li, J. Ye; D.A. Scott, A.L. Osterman, A. Sengupta, A. Weljie, M. Huang, D. Zhang, E. Radaelli, J.W. Tobias, F. Rambow, P. Karras, J.-C. Marine; X. Xu, A.G. Hatzigeorgiou, S. Ryeom, A.J. Diehl, S.Y. Fuchs, E. Puré and C. Koumenis. 2022. Nature Cell Biol. 24:940-953. PMID:35654839.
Loss of p19Arf Promotes Fibroblast Survival During Leucine Deprivation Enhancing Tumor Progression. Roby, K.C., Jr, A. Lieberman, B.J. Kim, N. Zaragoza Rodríguez, J.M. Posimo, T. Tsang, J. Verginadis3, E. Puré, D.C. Brady, C. Koumenis, S. Ryeom. 2022. Biology Open. 11: bio058728.
CAR T cells produced in vivo to treat cardiac injury. Rurik, J.G., I. Tombácz, A. Yadegari, P.O. Mendez Fernandez, S.V. Shewale, L. Li, T. Kimura, O.Y. Soliman, T.E. Papp, Y.K. Tam, B.L. Mui, S.M. Albelda, E. Puré, C.H. June, H. Aghajanian, D. Weissman, H. Parhiz and J. A. Epstein. 2022. Science. 375:91-96.
Activation of the p38α stress-activated protein kinase drives the formation of the pre-metastatic niche in the lungs. Gui, J., F. Zahedi, A. Ortiz,, C. Cho, K. Katlinski, K. Alicea-Torres, J. Li, L. Todd, D.P. Beiting, C. Sander, J.M. Kirkwood, B.E. Snow, A.C. Wakeham, T.W. Mak, J.A. Diehl, C. Koumenis, S.W. Ryeom, B.Z. Stanger, E. Puré, D.I. Gabrilovich and S.Y. Fuchs. 2020. Nature Cancer 1:603-619.
Fibroblast activation protein regulates lesion burden and the fibroinflammatory response in apoE-deficient mice in a sexually dimorphic manner. Monslow, J., L. Todd, J.E. Chojnowski, P.K. Govindaraju, R.K. Assoian and E. Puré. 2020. Amer. J. Pathology. 190:1118-1136. PMID: 32084369; PMCID: PMC7237832.
Deconstructing tumor heterogeneity: The stromal perspective. Vickman, R.E., D.V. Faget, P. Beachy, D. Bebee, N.A. Bhowmick, E. Cukierman, W.-M. Deng, J.G. Granneman, J. Hildesheim, R. Kalluri, K.S. Lau, E. Lengyel, J. Lundeberg, J. Moscat, P.S. Nelson, K. Pietras, K. Politi, E. Puré, R. Scherz-Shouval, M.H. Sherman, D. Tuveson, A.T. Weeraratna, R.M. White, M.H. Wong, E.C. Woodhouse, Y.Zheng, S.W. Hayward, S.A. Stewart. 2020. Oncotarget 11(40):3621-3632. PMID: 33088423. PMCID: PMC7546755.
Cancer-associated fibroblasts downregulate type I interferon receptor to stimulate intratumoral stromagenesis. Oncogene. Cho,C., R. Mukherjee, A.R. Peck, Y. Sun, N. McBrearty, K.V. Katlinski, J. Gui, P.K. Govindaraju, E. Puré, H. Rui and S.Y. Fuchs. 2020. 39(38):6129-6137. PMID:32807917. PMCID: PMC7502515.
A framework for advancing our understanding of cancer-associated fibroblasts. Sahai, E., I. Astaturov, E. Cukierman, D. DeNardo, M. Egeblad, R.M. Evans, D. Fearon, F.R. Greten, S.R. Hingorani, T. Hunter, R.O. Hynes, R.K. Jain, T. Janowitz, C. Jorgensen, A. Kimmelman, M. Kolonin, R. Maki, S. Powers, E. Puré, D. Ramirez, R. Scherz-Shouval, M.H. Sherman, S. Stewart, T. Tlsty, D. Tuveson, F.M. Watt, V. Weaver, A. Weeraratna and Z. Werb. 2020. Nat Rev Cancer. 20(3):174-186. PMID: 31980749 PMCID: PMC7046529.

Director, Puré Lab
Ellen Puré, PhD
Grace Lansing Lambert Professor, past Chair of Biomedical Sciences, and Professor of Systems Pharmacology and Translational Therapeutics
Join Us Today
Join us in our quest to transform the landscape of chronic disease understanding and treatment. Contact Ellen Puré, PhD, if you are interested in being a part of the lab.
Find Us
University of Pennsylvania School of Veterinary Medicine
Lab Address
Hill Pavilion, Room H430
380 S. University Ave
Philadelphia PA 19104-4539
Office
Hill Pavilion, Room 410E
380 S. University Ave
Philadelphia PA 19104-4539
Our Team

Allison Ardon
Khuloud Bajbouj, PhD

Leslie Hopper

Li Huang
Henry Utset
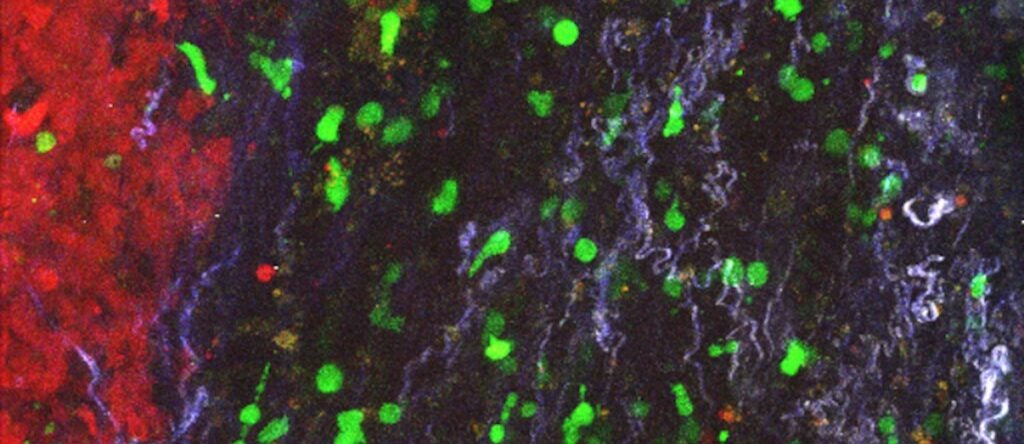
Removing the barrier surrounding solid tumors clears path for T cells (link is external)
Penn researchers uncover a new way to target solid tumors. Using CAR T cells to remove cancer-associated fibroblasts surrounding pancreatic tumors allows T cells to infiltrate and attack the tumor…
