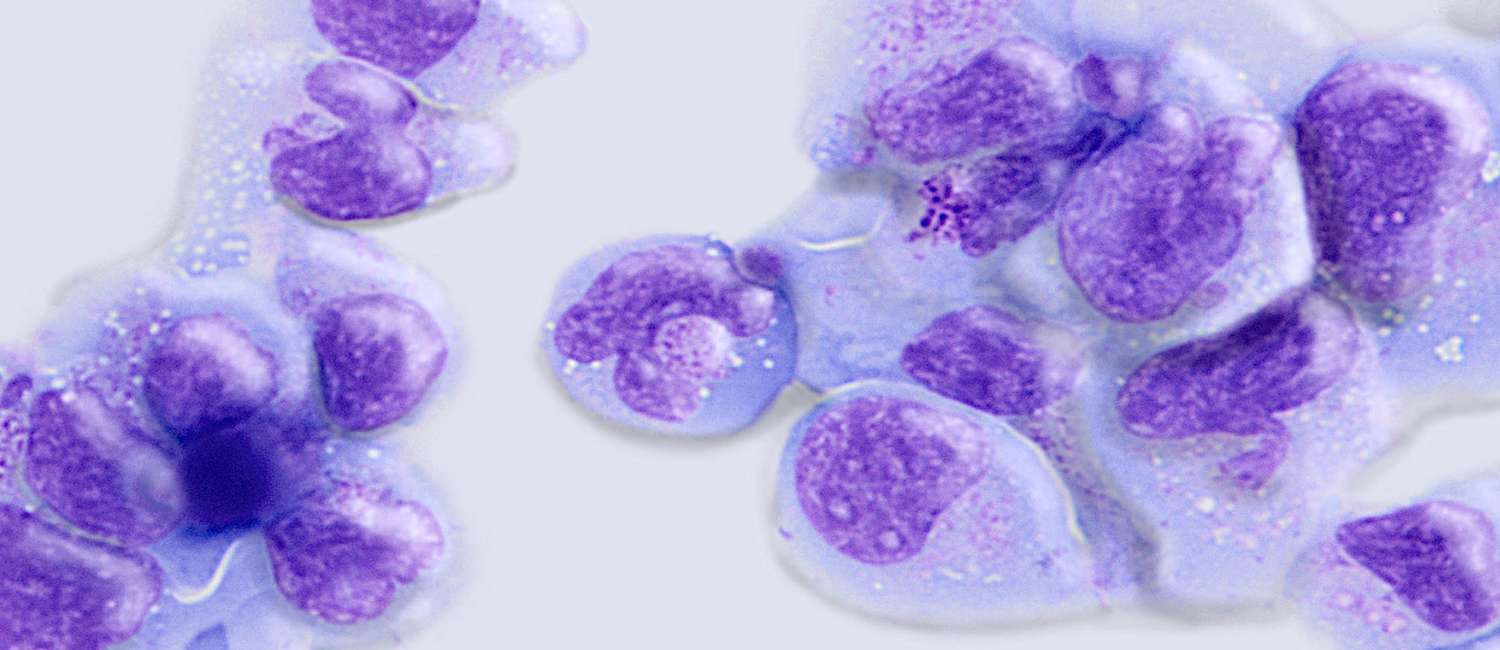
 Canine iNKT cells. (Image: Courtesy of Nicola Mason and Antonia Rotolo)
Canine iNKT cells. (Image: Courtesy of Nicola Mason and Antonia Rotolo)
Researchers from the School of Veterinary Medicine and Perelman School of Medicine have shown that invariant natural killer T cells from a healthy donor can persist in MHC-mismatched canines, demonstrating a reliable platform to inform human clinical trials.
Allogeneic invariant natural killer T cells (allo-iNKTs) from a healthy donor have been shown to have therapeutic effects in treatment-resistant cancers and improve survival from COVID-19-related acute respiratory failure in previous studies. Unlike T cells, allo-iNKTs can be transferred from one person to another without causing graft-versus-host disease. But allo-iNKT cells rapidly become undetectable in the body after infusion, raising concerns over their rejection and disease relapse. Their functioning also varies from person to person.
Researchers from the School of Veterinary Medicine and Perelman School of Medicine hypothesized that allo-iNKTs could combat their own rejection—without additional gene editing—if taken from donors with certain characteristics.
They decided to test this theory in healthy dogs. Pet dogs develop cancers that share similarities with human cancers, and both species receive some of the same cancer-fighting drugs. More common animal models in research are not relevant models in this case because they have different iNKT biology from humans.
In the study, “Unedited allogeneic iNKT cells show extended persistence in MHC-mismatched canine recipients,” published in Cell Reports Medicine, the team found remarkable similarities between human and canine iNKT cell biology. They also identified biomarkers from donor cells that indicate longer persistence in recipients and found that these optimal cells remained detectable 78 days after infusion, whereas previous trials showed iNKT cells becoming undetectable within two weeks.
Antonia Rotolo, research assistant professor of immunobiology at Penn Vet, explains that current strategies typically involve either using donor cells from an individual with the same major histocompatibility complex (MHC) proteins as the recipient or eliminating MHC proteins on the donor cell before transferring to the recipient, to reduce the risk of rejection. But this can make production of donor cells costly and time-consuming, and so it is significant that Penn researchers saw results in MHC-mismatched recipients.
“Now we have a fantastic, clinically relevant canine system in which to test hypotheses and therapeutic regimens that would be otherwise extremely difficult to bring to the patients,” Rotolo says. Since the dogs in this study were 30 kilograms, she says the protocol could be readily translated for pediatric patients.
She calls it “remarkable” that the iNKT cells remained functional for nearly three months. For a human cancer patient, Rotolo says, this extended longevity would mean reduced risk of relapse and longer therapeutic effect.
“The data we have generated using canine cells lay the groundwork for performing pre-clinical studies in canine patients with cancer and inflammatory diseases, which will inform the use of these cells in the human clinic,” says senior author Nicola Mason, professor of medicine and pathobiology at the School of Veterinary Medicine.
 Nicola Mason and Antonia Rotolo (Image: John Donges/School of Veterinary Medicine)
Nicola Mason and Antonia Rotolo (Image: John Donges/School of Veterinary Medicine)
The optimal donor
The researchers first found evidence that canine iNKTs share similar biological properties with human iNKTs. They then used single-cell RNA sequencing to identify iNKT molecular signatures from four healthy canine donors, which Mason says revealed the variability in molecular profiles from different donors.
One donor’s iNKT cells were “enriched in central memory signatures known to promote longer iNKT survival and anti-tumor activity,” the study states, and had significantly less exhaustion-related genes than the other donors. The team therefore generated clinical-scale iNKT cells from this donor and infused them into two healthy dogs.
“Both allo-iNKT-treated dogs showed a prompt increase in circulating lymphoid cells and early signs of peripheral lymphoid activation after allo-iNKT infusion, underscoring the safety of allo-iNKTs and their suitability for large dose infusions,” the study says. No adverse events were observed.
The paper also notes that this kind of donor- selection strategy is important because testing showed there are intrinsic iNKT features that chimeric antigen receptor (CAR) engineering cannot change.
In addition to demonstrating a reliable platform to inform human clinical trials, Mason says the research shows it is now possible to offer iNKT immunotherapy to pet dogs with cancer who do not have another viable therapeutic option.
Antonio Rotolo is a research assistant professor of immunobiology at the University of Pennsylvania School of Veterinary Medicine.
Nicola J. Mason is a professor of medicine and pathobiology at Penn Vet.
Other co-authors are Eoin C. Whelan, Matthew J. Atherton, Martina Piviani, Enrico Radaelli, and Raimon Duran-Struuck from Penn Vet, and Irina Kulikovskaya, Danuta Jarocha, Joseph A. Fraietta, Michele M. Kim, Eric S. Diffenderfer, and Keith A. Cengel from the Perelman School of Medicine.
This work was supported by the American Society of Gene and Cell Therapy, a Cayman Chemicals Women in Research grant, and funds from the National Institutes of Health (U24 supplement 4-U24-CA-224122-02, U01 CA272270-01, KO8CA252619, and P40-OD-010939).